4 Reasons a Lyme Test Will Come Back Negative Even If a Person Truly Has Lyme Disease
Don't Put 100% Trust in What is Not 100% Accurate
Depending on which study you consult, the current tests used to diagnosis Lyme disease are accurate only between 50-80% of the time, even with the best labs. IGeneX themselves, the most used and trusted lab by Lyme doctors and physicians for confirming a Lyme disease diagnosis, says, "Diagnosis should not be made on laboratory tests alone".
“It is important to note that a positive IgG and/or IgM Western blot only implies exposure to B. burgdorferi. It is only part of the test battery and is not confirmatory for Lyme disease. It does not mean the patient has Lyme disease; that is a clinical diagnosis.” -IGeneX source, 1998.
This exact current-day inaccuracy of Lyme testing in why the best Lyme physicians know not to rely upon laboratory testing for confirming a Lyme disease diagnosis solely, but to couple it with symptoms the patient experiences, and circumstantial evidence. It should be noted that there are labs out there that employ more advanced and modern techniques than others to increase the odds of obtaining a Lyme diagnosis. This article will talk about that later.
|
It exists, that a person can continuously test negative for Lyme disease, but still have an active Lyme disease infection. There are many reasons why a Lyme test can come back negative; even continuously and when different labs and types of testing are employed. This article will discuss 4 reasons, and they're not the only reasons, why a Lyme test can come back negative, even if that person has Lyme disease.
Reason 1: You Have a Different Strain of Borrelia Than the Strain of Borrelia the Test Looks For |
|
You’re feeling great one day, but on that same day you’re feeling good, you locate a tick behind your ear. The next day you’re in bed with a fever and a debilitating headache. It’s got to be something the tick transmitted, right? And it has to be Lyme disease because the symptoms say so.
Instead of waiting for your doctor’s appointment which is 2 days away, you take the initiative and head to the emergency room of your local hospital. By the by, it’s important to know that an emergency room, even the best in the world, can test you for Lyme disease and receive a negative result, even if you truly have Lyme disease because no Lyme test is currently 100% accurate.
You’re lying in the hospital bed with an extreme headache, the emergency room doctor tests you for Lyme disease, and after what seems like the world’s longest hour, your test results come back and they’re negative. Now, the emergency room doctor could then have easily dismissed Lyme as the cause of your debilitation symptoms and fever, but this is no ordinary emergency room doctor. He’s still calling for Lyme disease, and not because the test used may have been inaccurate, which it could have been and he should know that, no - he’s calling for another Lyme disease test but this test will check for a different species of Borrelia - Borrelia miyamotoi. You wait another hour, and the test comes back positive - you have your cause.
Aside from the inaccuracies that already plague even the best Lyme disease tests to date, they may only test for a certain kind of Borrelia specie. In the United States, most standard Lyme disease tests are only looking for Borrelia burgdorferi. In Europe, most standard Lyme tests are only looking for Borrelia garinii. To date, there are around 18 discovered species of Borrelia with attention focused on a select few.
Reason 2: The Lab Performing Your Lyme Disease Test
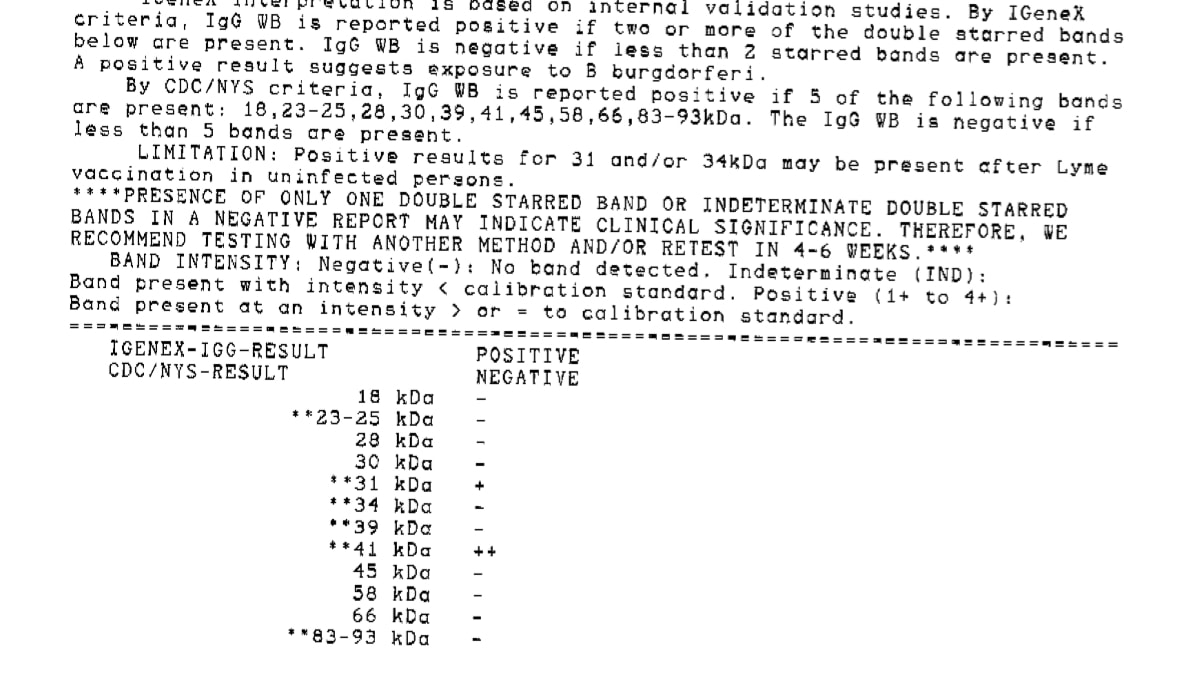
Not all labs for pathogen testing are the same, which means not all tests, in this instance, the western blot test, are the same. The western blot test is the most commonly used method for testing for Lyme disease. It tests for antibodies your immune system produced in response to the presence of Lyme bacteria. A western blot test performed at one lab can have a completely different protocol and technique for identifying Lyme antibodies than another lab performing a Western Blot test as well.
|
|
IGeneX is considered the go-to laboratory by Lyme doctors and physicians for testing a patient for Lyme disease with the western blot test. While the western blot test isn’t 100% accurate, and even IGeneX insinuates this, their methods and techniques used for identifying Lyme antibodies are more modern and advanced than other labs. For one example, they use a higher concentrated polyacrylamide gel “to get better separation of the important 31 kDa to 34 kDa antigens”. Having better separation of antigens allows a better discernment for identifying purposes. The 31 kDa (band) antigen is a major outer surface protein (OspA) of Borrelia burgdorferi. The 34 kDa (band) antigen is another outer surface protein (OspB) of Borrelia. Antibodies generated from these Borrelia antigens indicate not just a Lyme infection, but a late stage Lyme infection.
|
Having more modern and advanced techniques for testing for Lyme disease can increase the odds a person will receive a positive diagnosis if they do in fact have Lyme disease.
Reason 3: The Type of Test Used
There are quite a few methods for testing a person who is suspected of having Lyme disease. The most common testing methods for testing for Lyme disease include looking for the bacteria’s DNA in the blood (PCR or polymerase chain reaction), looking for antibodies the immune system produces in response to the Lyme bacteria’s presence (ELISA. or enzyme linked immunoassay, or western blot or western immunoblot), or looking for the bacteria itself (culture testing).
While these testing methods for Lyme disease can confirm a positive diagnosis, they can also yield negative results time and time again, even if a person truly have Lyme disease. The following information explains why the following types of tests can come back negative even if a person has Lyme disease:
PCR Test: This test looks for the presence of the Lyme bacteria’s DNA in blood to confirm a diagnosis. Your blood sample may not have any Lyme DNA in it because when Borrelia is in its cyst-form, it rarely releases any. Also, people with Lyme disease have periods of time where they are more or less symptomatic or asymptomatic, which is reflective of the bacteria’s activities. The PCR test can come back positive or negative depending on the activity level of the infection.
Antibody Test (Western Blot & ELISA): This test looks for antibodies the immune system produces after it comes into contact with the Lyme bacteria. This is the most commonly used method for testing for Lyme disease to date, and it works great if antibodies are being produced. Unfortunately, more times than not, a person can have Lyme disease, but no antibodies are being produced, which will produce a false negative (i.e., a person will test negative for Lyme even though they have it). There are many reasons why antibodies aren’t being produced when a person has an active Lyme infection, and here are a few:
- Cyst form of Borrelia: The Lyme bacteria can transform its physical state from a spirochete to a cyst. When it is in cyst form, it is not creating (i.e., synthesizing) any of its surface components (e.g., proteins) that the immune system needs to come in contact within in order to make antibodies
- Antibiotics: If a person is on antibiotics while they’re being tested for Lyme disease, their immune system may not be able to produce antibodies as well compared to being tested while not taking antibiotics.
- Testing too soon: The immune system needs a chance, if it even gets one, to produce antibodies in response to the presence of the Lyme bacteria. The part of the immune system that produces antibodies (the adaptive immune system) is activated roughly 4 to 7 days after the innate immune response is unable to initially destroy the foreign invader. In the case of Lyme disease, the Lyme bacteria has many ways to prevent the innate immune response from even activating and one example is the tick’s saliva. The innate immune response has three lines of defense before the adaptive immune system (antibody producing immune system phase) takes over. Part of the second line of defense for the innate immune response is the complement immune system. The complement immune system will kill the foreign invader if it is activated by one of three pathways: The classical pathway, the mb-lectin pathway, or the alternative complement pathway. The latter, the alternative complement pathway, is the pathway that deals specifically with Borrelia burgdorferi. The alternative complement pathway will trigger the complement immune response if complement protein C3b can bind to the surface of the spirochete. The tick’s saliva contains specific immune suppressing components that prevents this action from even occurring. So, as a result, the innate immune response is delayed or hindered, which allows the Lyme spirochete to take hold, and a possible delay in the adaptive immune response which is responsible for making antibodies.
- Type of antibody test: The ELISA test is less sensitive, meaning it doesn't produce enough of certain types of antibodies needed to identify the presence of the Lyme bacteria. While the western blot is much more sensitive at detecting other types of antibodies from the presence of the Lyme bacteria, which increases the odds of a positive diagnosis, even the western blot test can be performed differently (i.e., more or less sensitive) across different labs depending on the testing protocol the specific Lab employs.
|
Borrelia Culture Test: This test looks for the actual presence of the Lyme bacteria in a person’s blood. It completely skips the middle man, antibodies, of antibody testing, and is considered the closest test to 100% accuracy in detecting an active Lyme infection in a person. The problem with this test is that it relies on a living Lyme bacterium to be cultured (i.e., grown), and the nature of the Lyme bacteria is that it does not survive long outside of its host, even in cyst-form. This is why Advanced Laboratory Services, the lab that performs the Borrelia Culture Test, needs your blood sample within 24 hours of being withdrawn.
|
|
The current inaccuracies of Lyme disease testing is why any good Lyme doctor or physician will also take into account the symptoms a person suspected of having Lyme disease has, with laboratory testing, in order to make a clinical diagnosis.
Reason 4: You Don’t Have Lyme Disease, but a Co-infection
When you’re bit by a tick, you’re playing the lottery, as Scott Forsgren of betterhealthguy.com says. The tick you were bitten by could have a combination of infectious agents which include, but aren’t limited to, Lyme disease and a co-infection, just a co-infection, just Lyme disease, no infections at all, or a completely new specie of Borrelia or infection yet to be discovered.
For the sake of argument, you get tested for Lyme disease through one of the most reputable labs in the world for testing for Lyme. Why? Well, because you have symptoms that warrant such a test. And also for the sake of argument, let’s say this lab’s tests are 100% accurate at diagnosing Lyme disease (please note: currently no lab claims to be 100% accurate at diagnosing Lyme disease). One week later, your test results come back and they’re negative for Lyme. How is that possible? Even though this hypothetical lab is 100% accurate at diagnosing Lyme disease, and your symptoms greatly suggest Lyme, your lab work came back negative.
The overlooked answer to this enigma could possibly be a co-infection, or two, or more! Many of the co-infections that a person can receive through the same bite a tick can transmit Lyme disease, produce symptoms that can nearly mirror those symptoms of Lyme disease. You may have an overlooked co-infection, or two, and not Lyme disease.
Conclusion
If you, or someone you know, has a Lyme test performed and it comes back negative despite the empirical evidence of notable Lyme symptoms, and every other common protocol test for other diseases and ailments has been performed and yielded negative results, continue to consider the possibility that you may still have an active Lyme disease infection.
And even if your doctor tells you you’re negative for Lyme disease, but in your heart you still know it to be the case, find a doctor who knows the ins and outs of Lyme disease. But also be wary of doctors who claim to know how to treat Lyme disease, or accept chronic Lyme disease as reality, but are just in the practice for a quick, large buck.
|
|
Science is supposed to be consistent across the board, but in the case of chronic Lyme disease, there are doctors who acknowledge chronic Lyme disease, and there are those that don’t. You wouldn’t find a astrophysicist these days that didn’t know or won’t accept the moon rotates around the Earth. Both doctors and astrophysicists, despite their different fields, rely upon science as the tool, method, and process by which we as human beings obtain truth. Any inconsistencies in the acceptance of scientific evidence is the willful choice to remain ignorant - a price many with chronic Lyme disease currently pay.
|
Remember, just because Lyme tests aren’t 100% accurate, doesn’t mean they can’t be in any way accurate. It’s all about discretion of circumstantial evidence. If you have symptoms of Lyme disease and your lab results come back positive, have good reason to assume you have Lyme disease. If you have symptoms of Lyme disease, and your fifth test comes back negative also, still don’t rule out the possibility of Lyme disease. This article is in no way suggesting a complete avoidance of Lyme testing. What it suggests is to not have 100% complete trust in a Lyme test, especially when no Lyme test is claimed to be 100% accurate.
Resources
- Rubin, C. M. "The Global Search for Education: In Search of Solutions – Ticks."ILADS. International Lyme and Associated Diseases Society, 9 Feb. 2014. Web. 22 Apr. 2015.
- "Lyme Borrelia – How Many Strains Are There?" Lyme Disease NeoGen. N.p., 27 May 2013. Web. 22 Apr. 2015.
- "PATRIC::Borrelia::Genome List." PATRIC::Borrelia::Genome List. N.p., n.d. Web. 22 Apr. 2015.
- Engel, Meredith. "Rare Tick-borne Disease Found in New York Area." NY Daily News. N.p., 1 Aug. 2014. Web. 22 Apr. 2015.
- Vogan, Sue, and Dr. Garth Nicholson, MD. "Interview: Dr. Garth Nicholson, PhD, Bacterial Co-infections in Chronic Diseases." Public Health Alert. N.p., 1 Feb. 2007. Web. 22 Apr. 2015.
- "A Guide: The Diagnostic Dilemma of Lyme Disease." Lyme Research Alliance. N.p., n.d. Web. 22 Apr. 2015.
- Main, Emily, and Dr. David H. Newman, MD. "Do You Really Need That Antibiotic?" Rodale News. N.p., 06 Jan. 2011. Web. 22 Apr. 2015.
- Buhner, Stephen Harrod. "Borrelia Burgdorferi: A Potent Emerging Disease."Healing Lyme: Natural Prevention and Treatment of Lyme Borreliosis and Its Coinfections. Randolph, VT: Raven, 2005. 26. Print.
- Advanced Laboratory Services. "How Long Can Borrelia Burgdorferi Survive outside Its Host?" Message to the author. 24 Oct. 2014. E-mail.
- "The IGeneX Western Blot: Better by Design." IGeneX, Oct. 2003. Web. 22 Apr. 2015. <http://www.igenex.com/innovations3.pdf>.
- "An Understanding of Laboratory Testing." An Understanding of Laboratory Testing. IGeneX, Spring 1998. Web. 24 Apr. 2015. <http://www.igenex.com/labtest.htm>.
Also on Tired of Lyme
Refresh
Refresh
Subscribe to Tired of lyme!
Subscribe to Tired of Lyme's mailing list and get notified of new articles!



Comments